Stay Safe and Informed about Coronavirus Disease (COVID-19)
As the coronavirus disease (COVID-19) pandemic continues to impact communities across the U.S. and globally, the American Lung Association is monitoring recent developments, sharing new findings and providing guidance on how to protect yourself and your family from becoming infected and what to do if you become ill. You can trust us to share only science-based information for all Americans, including those with lung disease.
Please reference our Frequently Asked Questions from our Chief Medical Officer Dr. Albert Rizzo for updated, public health guidance. And we encourage you to hear directly from our national president and CEO in this important message.
COVID-19 Resources
Visit our COVID-19 disease section to learn:
- Signs and symptoms of COVID-19 and questions to ask your doctor.
- How to prevent COVID-19 and stop the spread.
- How COVID-19 affects people with existing lung disease.
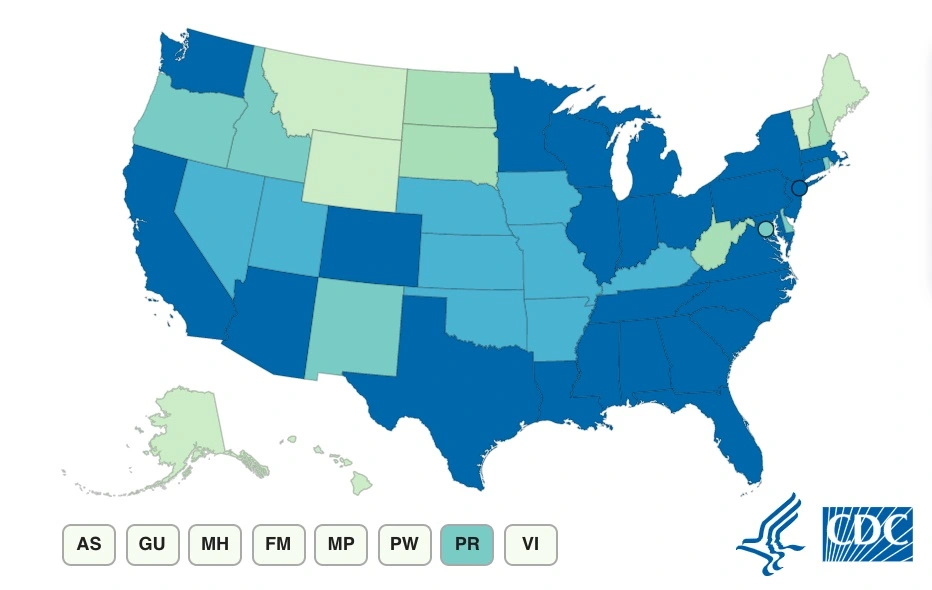
Keeping Track of COVID-19
See a map of the current cases and deaths reported in the U.S. and get connected to state health websites. View other data sources to help you understand the impact of COVID-19 in your area. View map.
What's New
COVID-19 Blog
Read our COVID-19 blog to learn more about topics in the news and important to you. We are talking to patients and caregivers as we navigate this pandemic together. We are sharing stories from healthcare providers who are supporting those affected by COVID-19. We are looking deeper at issues as they impact our daily lives. Read blog articles.
Keeping Your Chronic Condition Well Controlled
While individuals with chronic lung disease are not at higher risk for contracting COVID-19, they are more susceptible to severe complications if they do contract COVID-19. Keeping your lung disease well-controlled is an important factor to your overall health, especially now.
- If you are nervous about a visit to the doctor’s office, call to see if you can keep your regular appointments but have them over the phone or online.
- Continue to follow your Asthma Action Plan or COPD Action Plan.
- Consider mail order pharmacy options for your controller medications. And if your insurance allows, secure a 90-day supply of prescription medications.
- If you use a nebulizer to take inhaled medications at home, continue to maintain your regular medication schedule. Though, if you have suspected or diagnosed COVID-19, speak with your healthcare provider about additional precautions to take when using your nebulizer.
- Stay up-to-date on your vaccinations. Vaccines strengthen our immune systems and help keep you and those around you healthy.
- COVID-19 has also highlighted the importance of quality and affordable health insurance for patients. If you currently find yourself without health insurance, you can review some of your options here.
The important thing to remember is to stay the course when it comes to the long-term management of your chronic medical condition.
Disclaimer: The information in this article was medically reviewed and accurate at the time of posting. Because knowledge and understanding of COVID-19 is constantly evolving, data or insights may have changed. The most recent posts are listed on the EACH Breath blog landing page. You may also visit our COVID-19 section for updated disease information and contact our Lung HelpLine at 1-800-LUNGUSA for COVID-19 questions.
Blog last updated: August 21, 2023