Before a vaccine was introduced in the late 1940s, pertussis, more commonly known as whooping cough, was a leading cause of childhood illness and death in the United States. The vaccine was so effective that the number of cases in the U.S. went from more than a million diagnosed between 1940-1945, to less than 3,000 a year by the 1970s.
Since then, pertussis has again become increasingly common due to varied factors including improved diagnostic tests, more spread of the bacteria that causes pertussis, and waning immunity from current vaccines. In recent years several states have reported significant outbreaks, with most deaths occurring in babies younger than three months old.
To help protect yourself and your family from pertussis, here’s what you should know.
1. Whooping cough most commonly affects babies and young children but can affect anyone at any age.
While babies and young children are among the most affected, teenagers and adults are also at risk of becoming infected and spreading whooping cough. The bacteria that cause whooping cough, Bordetella pertussis, is spread easily from person to person through coughing and sneezing. Even if you have been vaccinated or are experiencing mild symptoms, you can spread whooping cough to others.
According to the Centers for Disease Control and Prevention (CDC), about one third of babies younger than one year old who contract whooping cough end up in the hospital. Young children are also at risk of other complications, such as pneumonia, pauses in breathing (apnea), and dehydration.
“The population at highest risk for severe complications are very young infants who are too small to get vaccinated against it, older adults, pregnant women and those who are immunocompromised,” Dr. Mora, CEO of Chicago Allergy Center, explained.
2. Pertussis is known for the distinct "whooping" sound made at the end of a coughing episode, giving it the name.
Although pertussis usually starts with typical cold-like symptoms, it is often not diagnosed until after one to two weeks, when the illness progresses from a mild cough into the second stage of persistent and rapid coughing spells. This stage is known as the paroxysmal stage.
The paroxysmal stage is categorized by violent coughing fits that often result in vomiting and is followed by a whooping sound. These coughing episodes may occur a few times a day up to several times an hour and are often worse at night and can interfere with sleep. This stage can last up to three months.
3. Vaccines are available to help prevent whooping cough across the lifespan.
“Pertussis complications can be severe, but there is a vaccine available. This is why everyone should get vaccinated against it and seek treatment early if they develop whooping cough symptoms, as we have good antibiotics to treat pertussis,” said Dr. Mora.
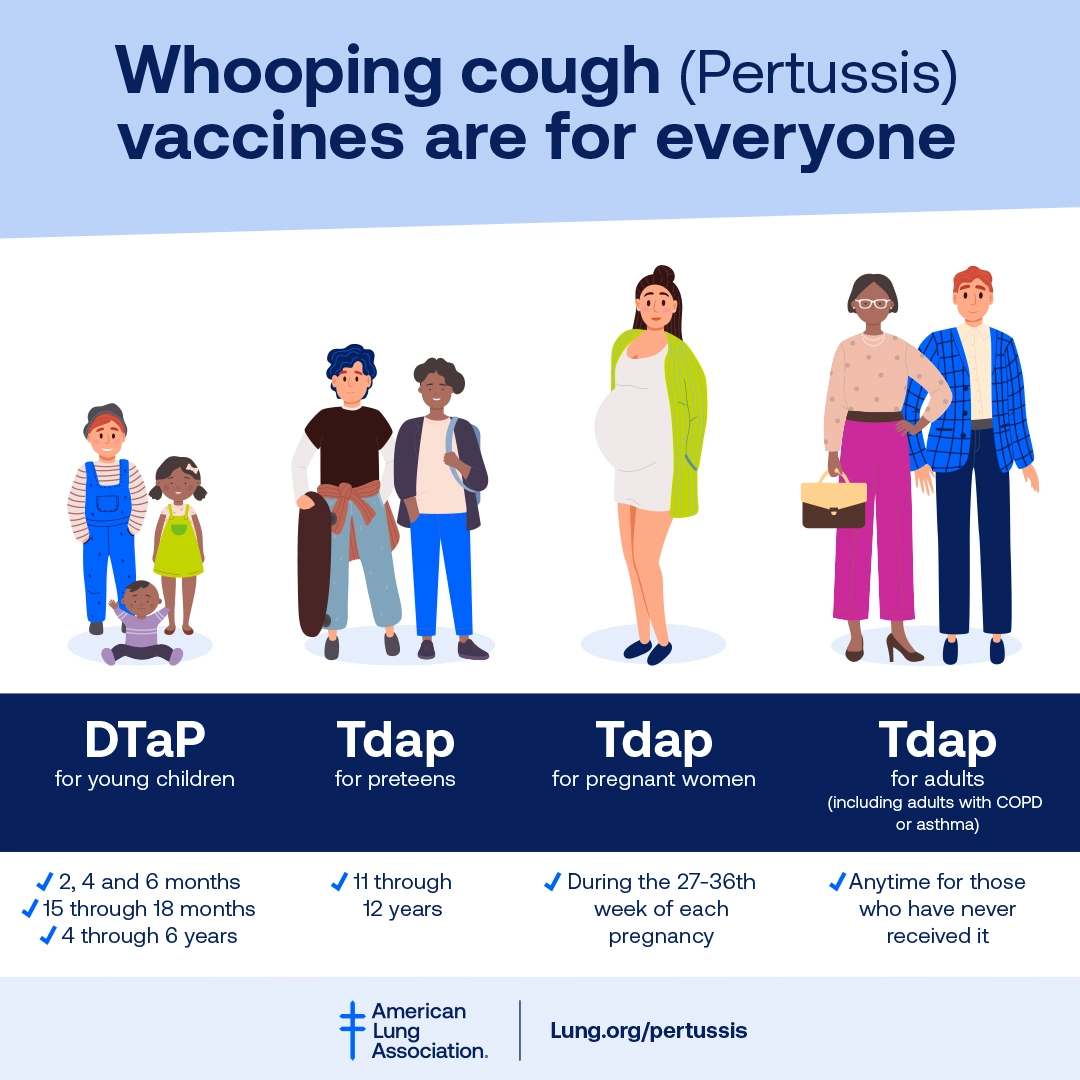
Vaccination is the best protection against pertussis. There are two types of vaccines to protect against whooping cough:
- DTaP to protect young children against diphtheria, tetanus, and pertussis.
- Tdap for use during pregnancy and to protect preteens through adults against tetanus, diphtheria, and pertussis.
Individuals who are pregnant can provide short-term protection for their babies by getting a Tdap vaccine during the 27th through 36th week of each pregnancy. Getting vaccinated during pregnancy lowers the risk of whooping cough in babies younger than two months old by almost 80%.
Children build their own immunity after birth through vaccination. For best protection against whooping cough, children need five doses of DTaP (diphtheria, tetanus, and acellular pertussis) vaccine by the time they are six. The CDC recommends the baby’s first dose beginning at two months old.
Preteens should get one shot of Tdap between the ages of 11 and 12 years to boost their immunity and adults who have never received a Tdap vaccine should get one as well.
Vaccines are effective, but not 100% effective. Vaccinated people who get whooping cough usually have more mild symptoms such as a cough that doesn’t last as long and coughing fits that are less common and severe.
4. The use of cough medications is typically not recommended in the treatment of whooping cough.
Antibiotics are the best way to treat pertussis. It is important that a doctor is seen as soon as possible, and treatment is started early to reduce severity and duration of the illness and the risk of spreading the infection to others.
Do not take over the counter cough medicine unless your healthcare provider recommends it for you.
Treatment after three weeks is unlikely to help because the bacteria are typically gone from your body despite still having symptoms. Coughing fits often persist for weeks because the bacteria have already caused damage.
5. There are several steps you can take for managing pertussis and reducing the risk of spreading it to others.
To start, see your doctor as soon as symptoms begin to occur and always follow the schedule for taking antibiotics exactly as prescribed. Try your best to keep your home free of any irritants that can trigger coughing, such as smoke, dust and chemical fumes. Use a clean, cool humidified mist to help loosen mucus and soothe the cough and practice proper handwashing. Drink plenty of fluids, including water, juices and soups, and eat fruits to prevent dehydration.
Although infection can occur throughout the year, be particularly cautious during the summer and fall months when pertussis cases tend to peak.“Our goal is to keep everyone healthy. This means increasing vaccination rates, practicing universal precautions, and diagnosing and treating early," Dr. Mora explained.
Those who have had an outbreak in their community should be especially vigilant about early symptoms. If you or someone in your household might have whooping cough, your best course of action is to contact your healthcare provider as soon as possible.
Blog last updated: September 9, 2024